Summary
🩺 Millions of women suffer from chronic pain—yet their symptoms are often dismissed or misdiagnosed.
🧬 Conditions like fibromyalgia, endometriosis, and autoimmune diseases are frequently overlooked due to gender bias in healthcare.
💡 This article explores the science, the stigma, and real-life stories behind this invisible epidemic—and what must change.
1. Introduction: When Pain Isn’t Believed
Chronic pain affects more than 50 million women in the U.S. alone. From migraines to endometriosis, fibromyalgia to interstitial cystitis, women are disproportionately impacted by conditions that are invisible, complex, and often misunderstood.
Yet many of these women face a double burden—not just the physical pain itself, but the psychological toll of not being believed. Studies show that women are more likely to be told their pain is “emotional,” “exaggerated,” or “stress-related” compared to men presenting similar symptoms.
This blog dives deep into how chronic pain manifests differently in women, why the healthcare system still lags behind, and what patients, providers, and policymakers can do to turn the tide.
2. Common Chronic Pain Conditions in Women 🔍
Women report chronic pain at significantly higher rates than men. Key conditions include:
- Endometriosis – affects ~1 in 10 women; takes an average of 8–10 years to be diagnosed
- Fibromyalgia – widespread pain with fatigue and cognitive issues; 80–90% of patients are women
- Interstitial Cystitis (Bladder Pain Syndrome) – recurring pelvic pain without infection
- Temporomandibular Joint Disorder (TMJ) – jaw pain, headaches, and tension; more common in women
- Chronic migraine – hormonal influences contribute to higher female prevalence
- Autoimmune diseases – 80% of autoimmune patients are women (e.g., lupus, rheumatoid arthritis)
These conditions often present with overlapping symptoms, making diagnosis complex and prone to dismissal.
3. The Gender Bias in Pain Diagnosis ⚠️
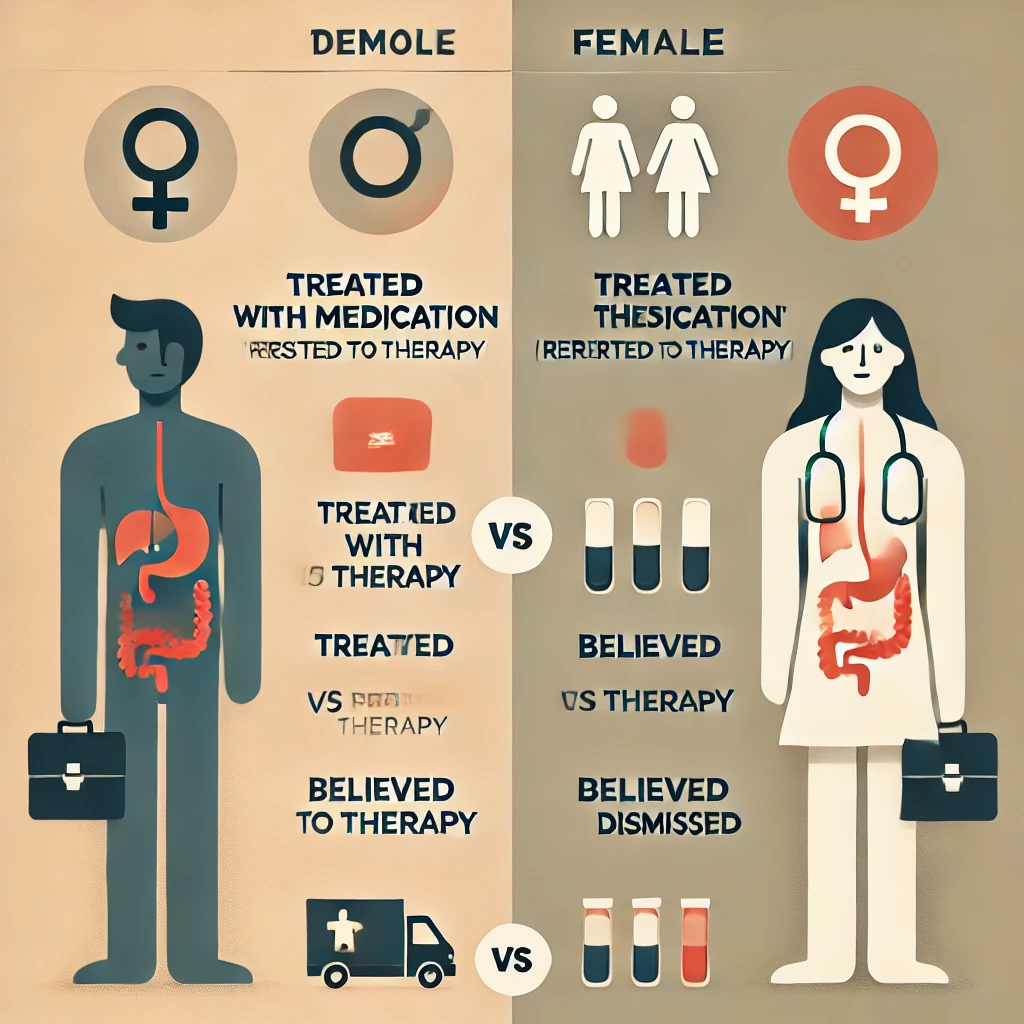
Numerous studies highlight a persistent gender gap in how pain is treated:
- Women are less likely to be prescribed pain medications than men for the same symptoms.
- Female pain is more likely to be labeled psychosomatic or linked to anxiety.
- Men’s pain is typically addressed with biomedical treatments; women’s pain, with psychological referrals.
- Women of color face even greater diagnostic delays and dismissal.
This bias is rooted in outdated medical models and cultural beliefs that see women as "emotional" or "dramatic," rather than credible narrators of their symptoms.
4. Expert Voices: Doctors and Patients Speak Out 👩⚕️🧑⚕️
Dr. Olivia Grant, Rheumatologist:
"When women come in describing vague, diffuse pain, many colleagues think depression—not inflammation. We’re trained to pathologize women’s emotions before we assess their physical reality."
Dr. Marissa Chen, Pain Management Specialist:
"We need to update diagnostic criteria and bias training. Fibromyalgia, for example, is still considered ‘controversial’ in many circles—but it’s a real, neurobiological condition."
Danielle R., 32, diagnosed with endometriosis after 11 years:
"I was told it was anxiety, stress, even my imagination. It took over a decade, three ER visits, and switching doctors five times to finally get a laparoscopy and a diagnosis."
Tasha M., 27, living with fibromyalgia:
"People assume I’m lazy or just depressed. I’ve had to ‘perform’ my pain to be taken seriously, and that performance is exhausting."
Dr. Grant:
"We need to ask different questions, listen more, and validate what we hear. Women don’t need to be more convincing. We need to be better doctors."

5. The Economic and Emotional Toll 💸🧠
Chronic pain in women comes at an immense cost—not only to individual well-being, but to healthcare systems and society as a whole.
Financial Costs:
- Loss of income due to missed work or disability
- Repeated visits to specialists, ERs, and therapists
- Out-of-pocket spending on alternative therapies
Emotional Costs:
- Medical gaslighting and trauma
- Depression, isolation, and reduced self-worth
- Strained relationships and social withdrawal
When pain is chronic and misunderstood, it becomes more than a medical issue—it becomes a life-altering experience.
6. What Needs to Change: Advocacy, Education & Equity 📣
Key Areas for Improvement:
- Medical education reform – Include chronic pain and sex/gender differences in training
- Funding female-focused research – Historically underfunded areas like endometriosis need priority
- Inclusive clinical trials – Ensure women are equally represented in all phases
- Listening-centered care – Encourage empathy, longer appointments, and shared decision-making
- Better insurance coverage – For physical therapy, mental health, and integrated care
Healthcare that truly serves women must recognize their pain as real, worthy, and treatable.

7. FAQ: Chronic Pain in Women ❓
❓ Why do women experience more chronic pain than men?
Research suggests hormonal differences, autoimmune predispositions, and pain processing mechanisms in the brain contribute. Social expectations may also cause women to report pain differently—or mask it.
❓ Why is it so hard to get diagnosed?
Because many chronic pain conditions present without visible damage on scans or blood work. Combined with implicit gender bias, this leads to years of dismissal before proper evaluation.
❓ Are women’s pain conditions under-researched?
Yes. Conditions like fibromyalgia, endometriosis, and chronic fatigue syndrome receive less than 5% of what similar male-dominant conditions receive in NIH funding.
❓ What should I do if I feel my doctor isn’t listening?
- Keep a symptom journal and bring it to appointments
- Ask specific questions and request documentation
- Get a second (or third) opinion if needed
- Seek out women-centered or integrative clinics
🩺 Chronic Pain Self-Assessment (For Women)
❓ How can partners and families help?
- Believe the patient—don’t minimize their experience
- Assist with daily tasks when needed
- Offer emotional support and attend appointments if invited
- Educate themselves about the condition
❓ Are alternative therapies useful?
Yes, especially when integrated. Options like acupuncture, gentle movement (e.g., yoga), cognitive behavioral therapy (CBT), and anti-inflammatory nutrition can improve outcomes.
❓ Can chronic pain improve or go away?
In some cases, yes. With the right diagnosis, targeted treatment, and lifestyle adjustments, many women experience significant symptom reduction. But it requires being taken seriously early.
❓ What are the long-term risks of untreated pain?
Untreated chronic pain can lead to nervous system sensitization, mobility loss, mental health decline, and even permanent disability.
❓ Is it all in my head?
Absolutely not. Chronic pain is a real physiological process—often involving inflammation, neurotransmitter dysregulation, and immune dysfunction. Psychological symptoms may arise as a result, not a cause.
❓ Where can I find support?
- Online communities (e.g., Reddit’s r/fibromyalgia, Endometriosis Foundation of America)
- Pain support groups (virtual and in-person)
- Specialized pain clinics or women’s health centers
- Mental health professionals familiar with chronic illness

8. Final Thoughts: Listening Is the First Treatment 🎙️
Chronic pain in women is not invisible—it’s just being ignored.
By listening better, funding smarter, and treating more holistically, we can turn the tide. It’s time for healthcare systems, families, and society to believe women, respect their voices, and deliver the care they deserve.
Because every woman in pain deserves to be heard—and healed.
💬 Have you or someone you love experienced chronic pain that was overlooked or misunderstood?
Join the conversation, share your story, and let’s create a system that finally listens. 👇



