🔍 TL;DR (3-Sentence Summary)
- Ultraprocessed foods (UPFs) are being increasingly linked to mood disorders like depression and anxiety through pathways involving inflammation, gut dysbiosis, and neurochemical disruption.
- While once considered only a weight and metabolic issue, the brain-gut-immune axis reveals how UPFs may directly impact cognition, mood, and mental clarity.
- Reducing UPF consumption and supporting gut health may be one of the most effective lifestyle interventions for protecting long-term emotional well-being.
🎙️ Moderator (Sasha Lee, Nutritional Neuroscience Writer):
Welcome to Brain & Bite, where we decode the science behind food and mood. Today’s hot-button topic: Are ultraprocessed foods quietly sabotaging our mental health?
Joining me are two experts:
- Dr. Leo Martínez, psychiatrist specializing in nutritional psychiatry
- Dr. Rina Caldwell, microbiome researcher and gut-brain axis specialist
🧠 Topic 1: What Are Ultraprocessed Foods (UPFs)?
Sasha: Dr. Martínez, can we start by defining UPFs?
Dr. Martínez:
Absolutely. UPFs are industrial formulations made mostly from substances extracted or synthesized from foods — like high-fructose corn syrup, flavor enhancers, seed oils, emulsifiers, and artificial colors. Think of packaged snacks, soda, instant noodles, frozen pizza — anything designed for hyper-palatable, long shelf life with low nutritional value.
Dr. Caldwell:
What makes them concerning is that UPFs often bypass our body’s natural satiety signals. They trigger dopamine spikes, contribute to poor microbiome diversity, and leave behind low-grade inflammation. That’s a dangerous combination when it comes to brain health.

Alt text: “Infographic showing examples of common ultraprocessed foods and their typical additives”
🌪️ Topic 2: How UPFs Impact the Brain
Sasha: We usually hear about UPFs and obesity. How do they affect the brain?
Dr. Martínez:
New studies show that UPFs can disrupt neurotransmitter balance, especially serotonin and dopamine. This isn’t just about willpower — it's about biochemical hijacking.
Dr. Caldwell:
UPFs alter the gut microbiome, which affects gut-brain communication. Poor microbial diversity is associated with higher levels of stress hormones and lower production of calming neurotransmitters like GABA.
Dr. Martínez:
Also, chronic consumption is linked to neuroinflammation — a key driver of brain fog, low motivation, and even depressive symptoms.
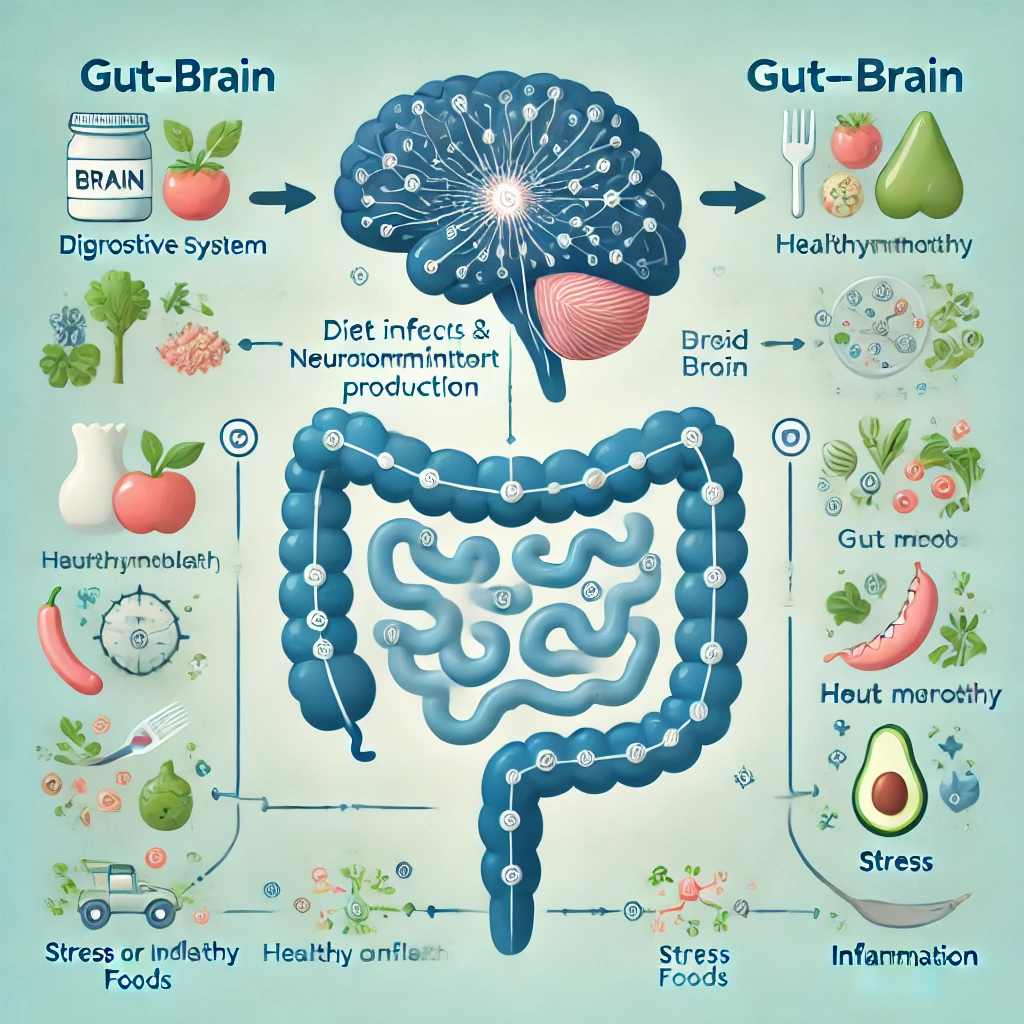
Alt text: “Diagram of gut-brain axis showing how diet influences mood and neurotransmitter production”
🔬 Topic 3: The Inflammatory Connection
Sasha: So inflammation is the key mechanism?
Dr. Caldwell:
Yes. UPFs contribute to systemic inflammation by increasing intestinal permeability (aka ‘leaky gut’) and introducing pro-inflammatory compounds. These molecules can cross the blood-brain barrier and interfere with neuronal function.
Dr. Martínez:
In psychiatry, we now see depression not just as a chemical imbalance, but as a neuroimmune disorder for many individuals. Dietary inflammation is part of that picture.

Alt text: "Visual flowchart showing how ultraprocessed foods (UPFs) can lead to leaky gut, systemic inflammation, neuroinflammation, and ultimately mood disorders such as depression and anxiety. Arrows connect each stage to emphasize the cascading biological effects. Designed for mental health and nutritional education."
🧩 Topic 4: Who’s Most at Risk?
Sasha: Is this more dangerous for some people?
Dr. Caldwell:
Children, teens, and women appear especially vulnerable due to hormonal changes and developing microbiomes. People with autoimmune conditions, ADHD, or high stress levels also show stronger responses to dietary triggers.
Dr. Martínez:
Let’s not forget low-income communities — where UPFs are often more affordable and accessible than whole foods. This creates nutritional inequality, which can compound mental health disparities.

Alt text: "Infographic highlighting demographics most vulnerable to ultraprocessed food-related mental health issues, including children, teenagers, women, individuals with autoimmune conditions, and low-income communities. Designed to visually represent health disparities linked to dietary patterns."
🌱 Topic 5: What Can We Do?
Sasha: Let’s talk solutions. How do we protect our brains?
Dr. Caldwell:
Start with small swaps: Replace one UPF a day with a whole food. Add prebiotic fibers, fermented foods, and polyphenols to support the microbiome.
Dr. Martínez:
I also recommend food journaling to track emotional responses to certain meals. Building awareness is step one.
Dr. Caldwell:
Don’t underestimate nature exposure, good sleep, and movement — they all reduce inflammation and strengthen the gut-brain axis.

Alt text: "Checklist-style infographic showing practical ways to support mental health through diet and lifestyle, including whole food swaps, gut-friendly nutrients, hydration, regular sleep, movement, and mindfulness. Designed for readers seeking simple and science-backed self-care strategies."
❓ FAQ: Ultraprocessed Foods & Mental Health
🍭 Q1: Are all processed foods bad?
A: No. Lightly processed foods like frozen vegetables or canned beans can be part of a healthy diet. The concern is with ultraprocessed items full of additives and stripped of fiber or nutrients.
🧠 Q2: Can quitting UPFs improve my mood?
A: Many report better clarity, focus, and emotional stability within weeks of reducing UPFs — but results vary based on individual biology.
👩🍳 Q3: Is this only an issue for people with mental illness?
A: Not at all. Even subclinical symptoms like low energy, poor focus, or irritability can be tied to diet quality.
🧃 Q4: Are diet sodas considered UPFs?
A: Yes. Most diet sodas contain synthetic sweeteners and other additives that can disrupt gut health and neurochemical balance.
🥦 Q5: Do I have to eat “perfect” to feel better?
A: No. The goal is progress, not perfection. Even 20–30% reduction in UPFs can yield measurable benefits.
💬 Have you noticed how food affects your mood and focus? Share your story — it might help someone else reconnect with their body and mind.



